Abstract
Introduction & Objectives: Endothelium activation by cancer cell derived MPs (CaCe-dMP) is essential in pathogenesis of cancer associated thrombosis (CAT). Recent studies demonstrated that exposed endothelial cells to CaCe-dMP acquire a new procoagulant phenotype characterized by endocytosis of tissue factor (TF) and enhancement of thrombin generation.
The aim of the present study was to investigate whereas the procoagulant properties acquired upon exposure of endothelial cells to CaCe-dMP are transferred to daughter generations of the endothelial cells.
Materials & Methods: Pancreas adenocarcinoma cells (BXPC3) and human breast cancer cells (MCF7) were cultured in 75 cm2 culture flasks at 37˚C in a 100% humidified atmosphere with 5% CO2 and were used for experiments at a confluence of 70%. Microparticles released in conditioned medium from BXPC3 and MCF7 cells were isolated by differential centrifugation. The pellets were washed twice and re-suspended in 1 ml endothelium cell basal medium (EBM-2). Human umbilical vein endothelial cells (HUVEC) were cultured for 72 h in the presence or absence of CaCe-dMP (mother generation : C0). Subsequently, they were washed and re-cultivated over three cycles to get daughter cell generations (Daughter Generations : C1, C2, C3). Tissue factor activity (TFa) was assessed with a chromogenic assay in the absence or presence of cells in normal PPP. Procoagulant phospholipid-dependent clotting time (Proag-PPL): was measured with STA®Procoag-PPL assay. Thrombin generation was studied as described elsewhere using Calibrated Automated Thrombogram®. All assays were from Diagnostica Stago (Asnières, France).
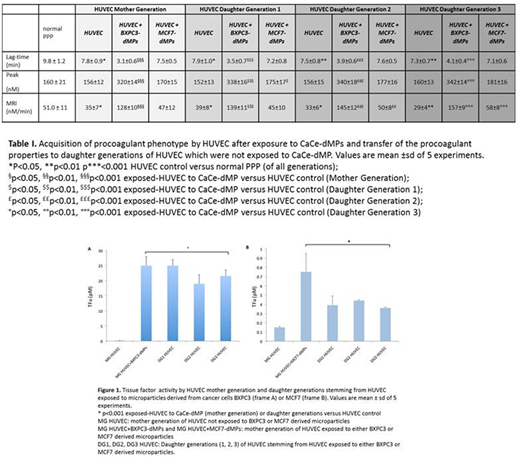
Results: The HUVEC and their microparticles manifested faint amounts of TFa (0.18±0.03 pM and 1.2±1.0 pM respectively). At steady state, HUVEC did not induce any detectable thrombin generation. Abundant TFa was showed by BXPC3-dMP (92±50 pM). The levels of TFa were significantly lower at MCF7-dMP (12.1±2.2 pM; p<0.05). Following exposure to BXPC3-dMP, the HUVEC abundantly displayed TFa as compared to non-exposed cells (25±3 pM versus 0.18±0.03 respectively; p<0.001) and showed significantly shorter Procoag-PPL® as compared to non-exposed cells (56±2 sec versus 102±10 sec. respectively ; p<0.001). HUVEC exposed to MCF7-dMP showed significantly increased TFa as compared to non-exposed cells (0.75±0.2 pM versus 0.18±0.03 respectively; p<0.001) and reduced the Procoag-PPL® clotting time as compared to non-exposed cells (65±3 sec versus 102±10 sec respectively; p<0.001). HUVEC exposed to CaCe-dMP significantly increased thrombin generation as compared to non-exposed HUVEC. Data of thrombin generation experiments are summarized in Table 1.
Daughter HUVEC from mother cells exposed to CaCe-dMP exhibited significantly higher TFa as compared to daughter generations from HUVEC non-exposed to CaCe-dMPs. The high TFa was conserved in three generations of cells derived from those exposed to CaCe-dMPs (Figure 1). Daughter generations of HUVEC exposed to CaCe-dMP induced significantly higher thrombin generation as compared to that induced by daughter generations of non exposed HUVEC (Table 1). The TFa of daughter cells stemming from HUVEC exposed to BXPC3 was significantly higher as compared to that of daughter cells stemming from HUVEC exposed to MCF7 (Figure 1). The Procoag-PPL® did not significantly change in daughter HUVEC exposed to microparticles derived either from BXPC3 or MCF7.
Conclusion: Upon exposure to CaCe-dMP, endothelial cells acquire a procoagulant phenotype marked by abundant TFa and enhanced thrombin generation potential. The procoagulant properties are transferred to the daughter generations of cells. These results support the concept that CaCe-dMPs lead to a procoagulant shift of endothelial cells which, upon exposure, present high TF activity and enhance thrombin generation. The procoagulant shift of endothelial cells can be transferred to next generations of endothelial cells and could be an additional mechanism - together with cancer-induced blood hypercoagulability - in the pathogenesis of cancer associated thrombosis.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal